Research
Ongoing Research
Trauma NB not only has a mandate to increase research capacity, but is also actively engaged in conducting research. Here are some projects that Trauma NB currently has on the go:
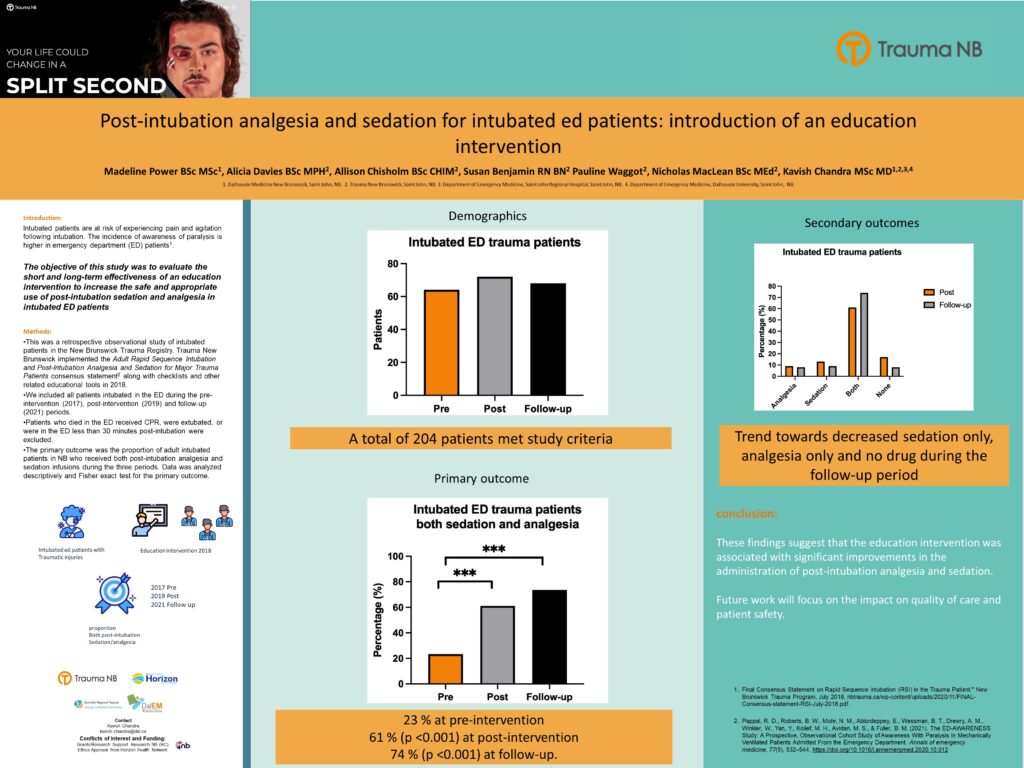
Falls and Seriously Injured Patients in New Brunswick: A Nine-Year Registry Review.
Motor Vehicle Crashes and Seriously Injured Patients in New Brunswick
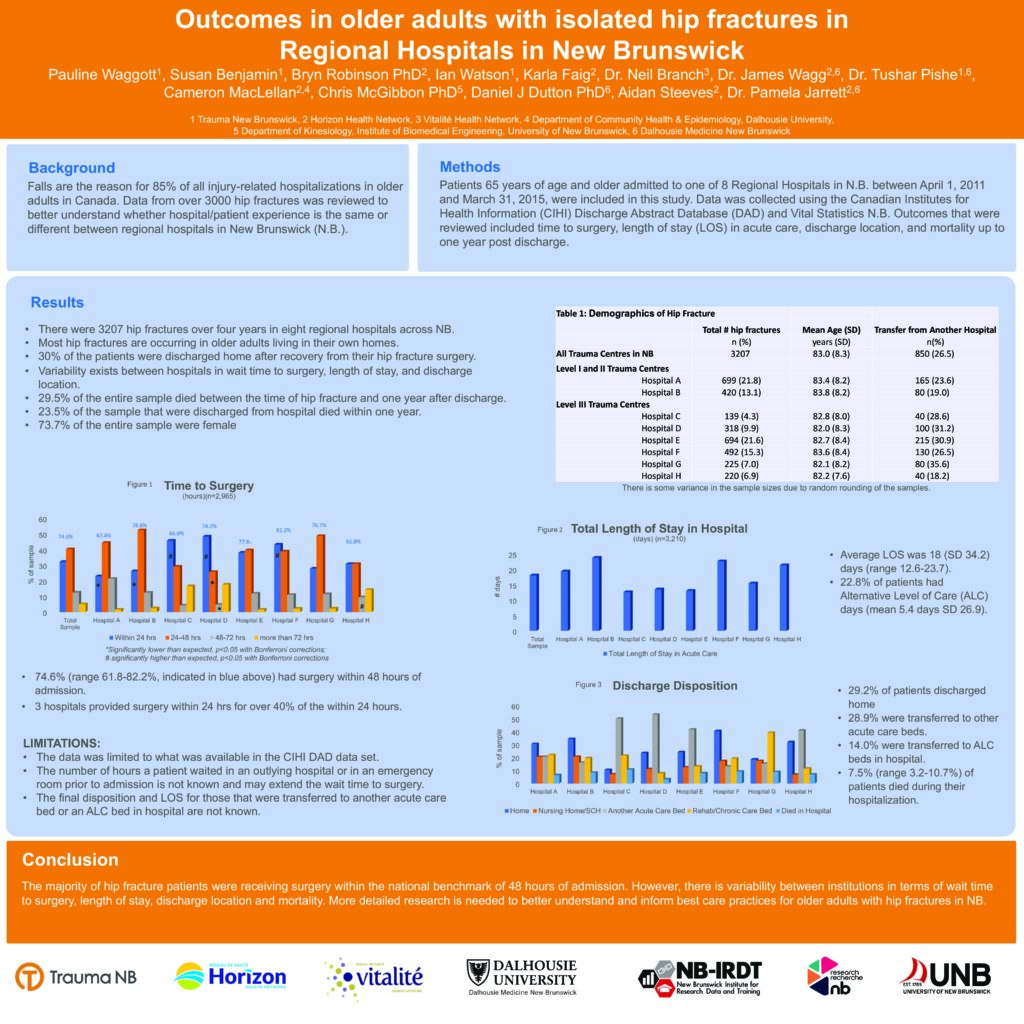
Post-intubation Analgesia and Sedation for Injured Patients in the Emergency Department: Introduction of an Education Intervention
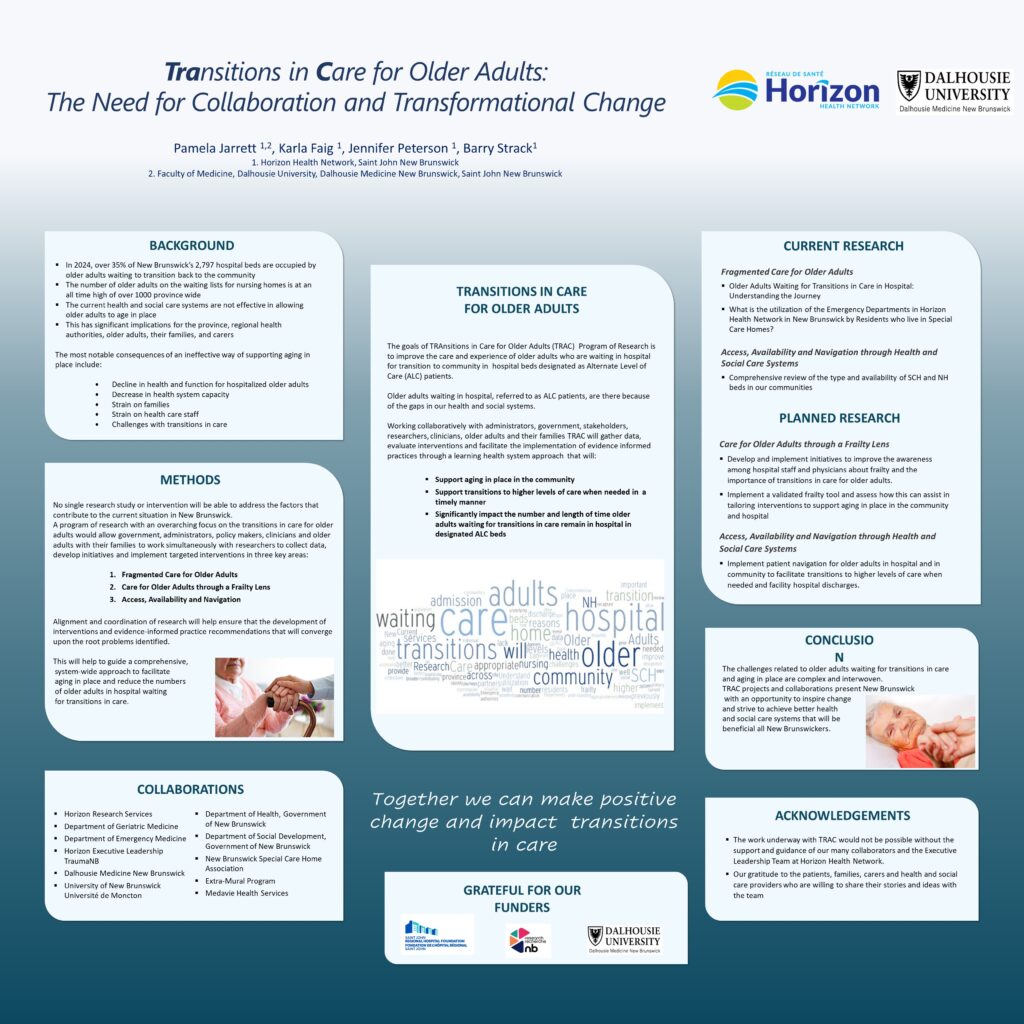
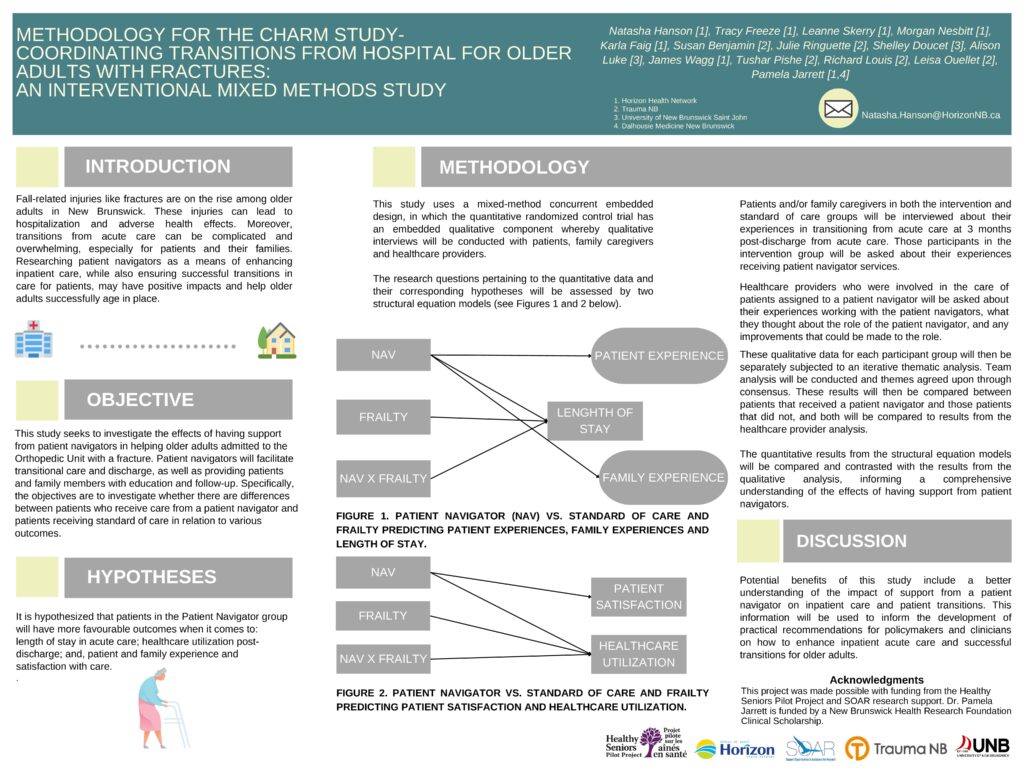
Supporting Older Adults through Transitions in Care: How Patient Navigators Can Help
Older Adults Waiting for Transitions in Care in Hospital: Understanding the Journey
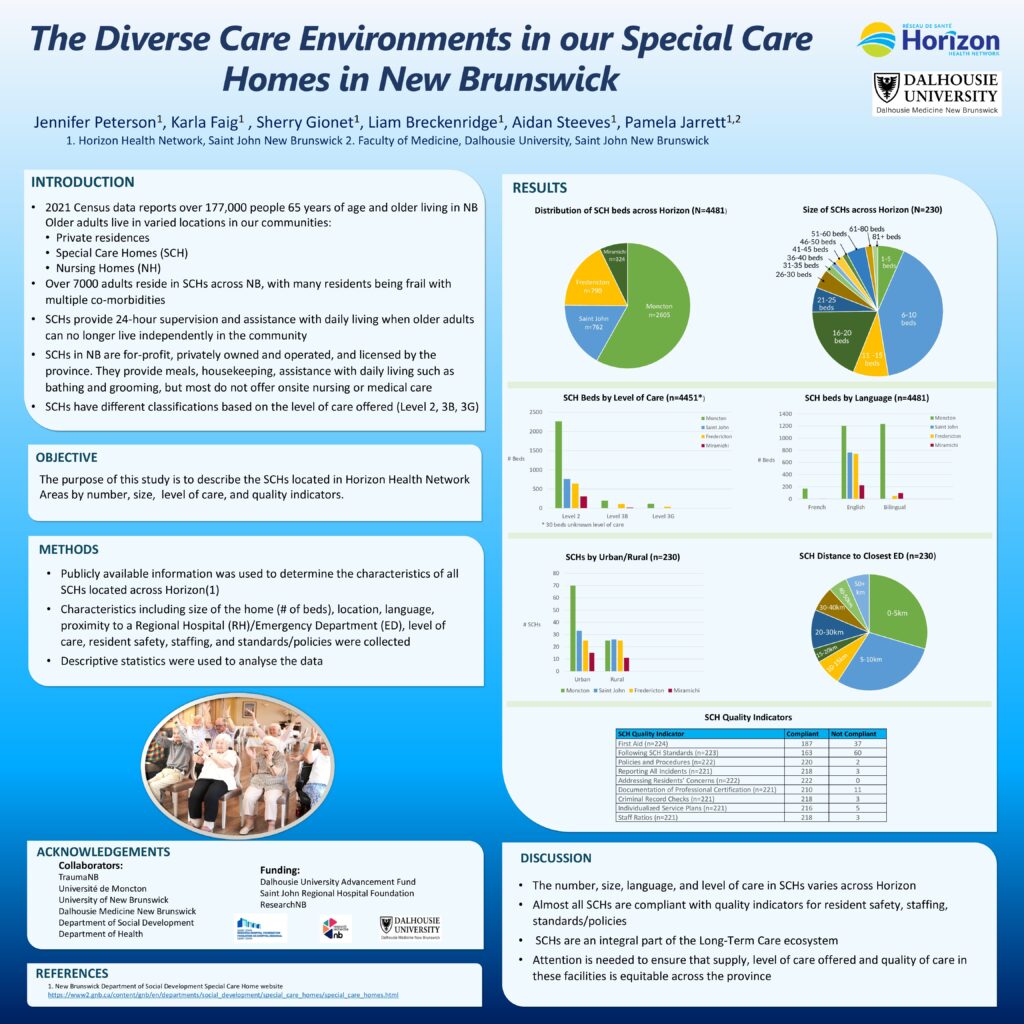
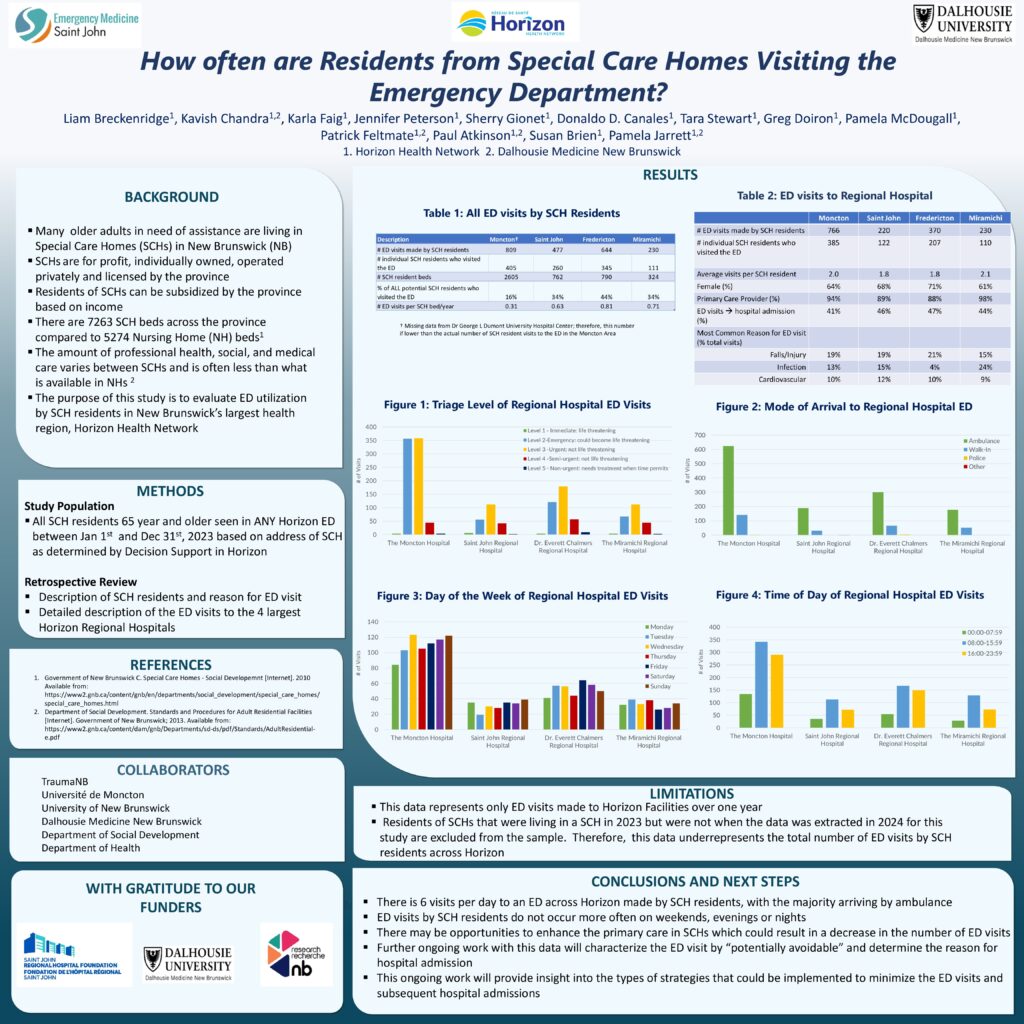
What is the utilization of the Emergency Departments in Horizon Health Network in New Brunswick by Residents who live in Special Care Homes?

Support for Researchers
Trauma NB is invested in increasing capacity for Trauma Research in New Brunswick. Trauma NB Research Subcommittee provides strategic oversight for research within the Program, with a particular focus on the descriptive epidemiology of trauma in New Brunswick. For further information please contact Allison.Chisholm@HorizonNB.ca
External Research Support:
For research policies, we follow those of the Horizon and Vitalité Regional Health Authorities. For more information, click the following links or contact Horizon Research directly at researchservices@horizonnb.ca or Vitalité Research directly at Recherche.Research@vitalitenb.ca
Research capacity in New Brunswick is growing, and there are a number of groups that promote local research. Below are external groups with a New Brunswick research focus.
Published Research
Click on the works below to access research published by members of Trauma NB:
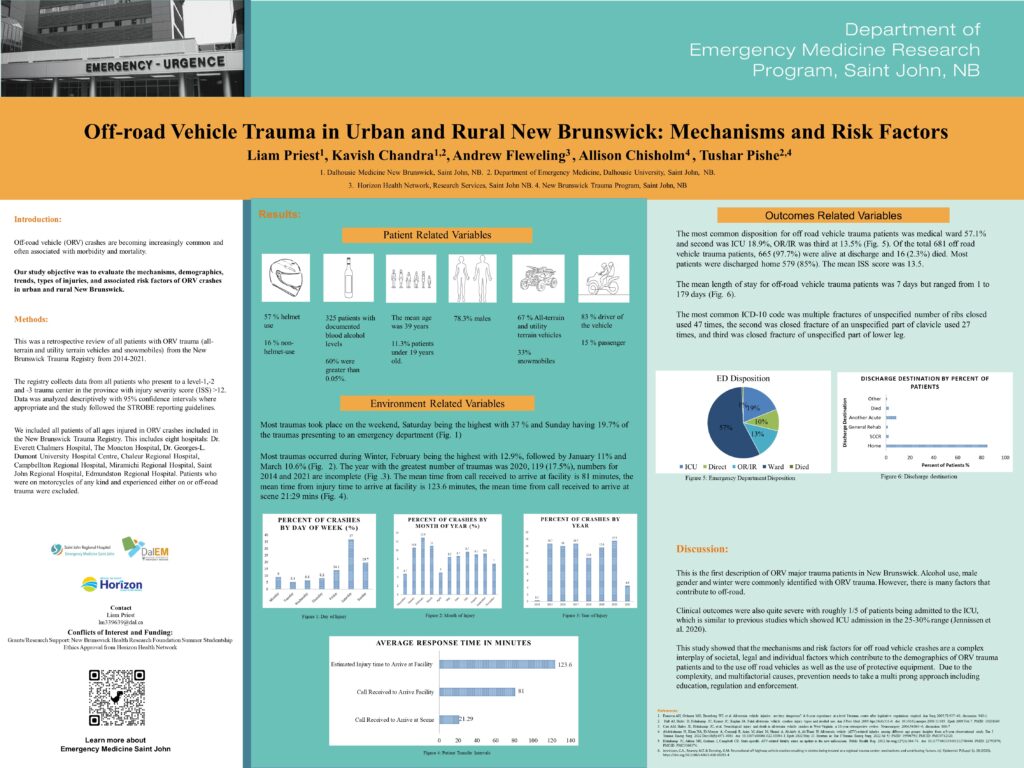
Priest L, Flewelling A, Atkinson P, et al. (March 13, 2025) A Multi-year Review of Major Off-Road Vehicle Injuries and Deaths in New Brunswick.
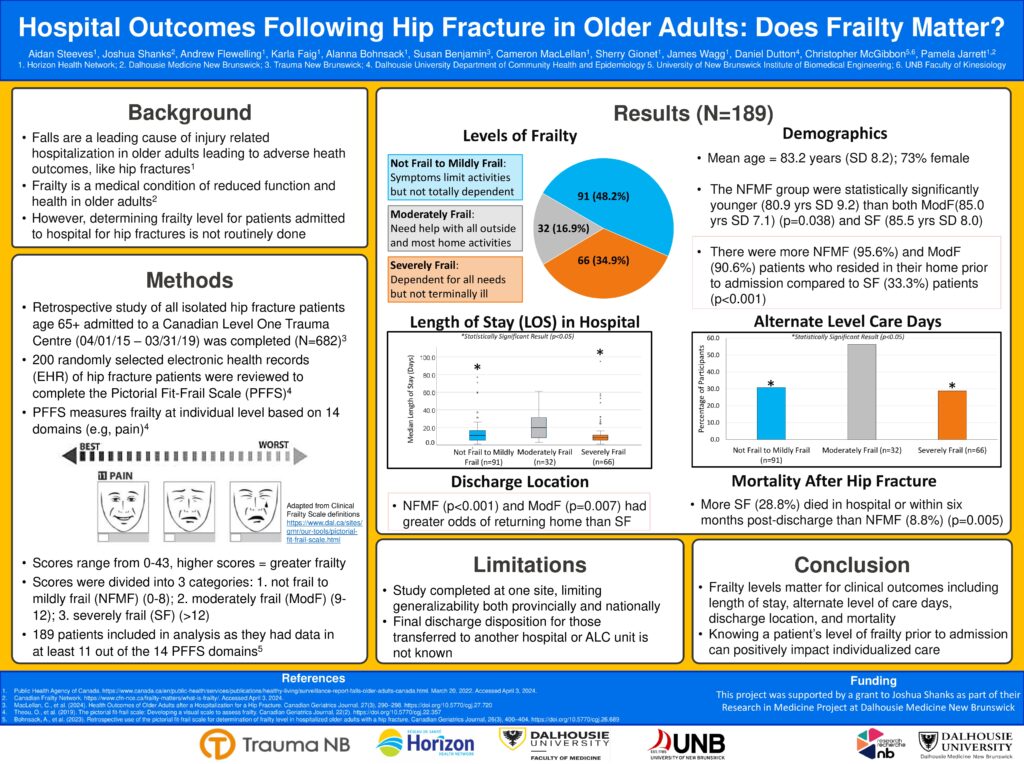
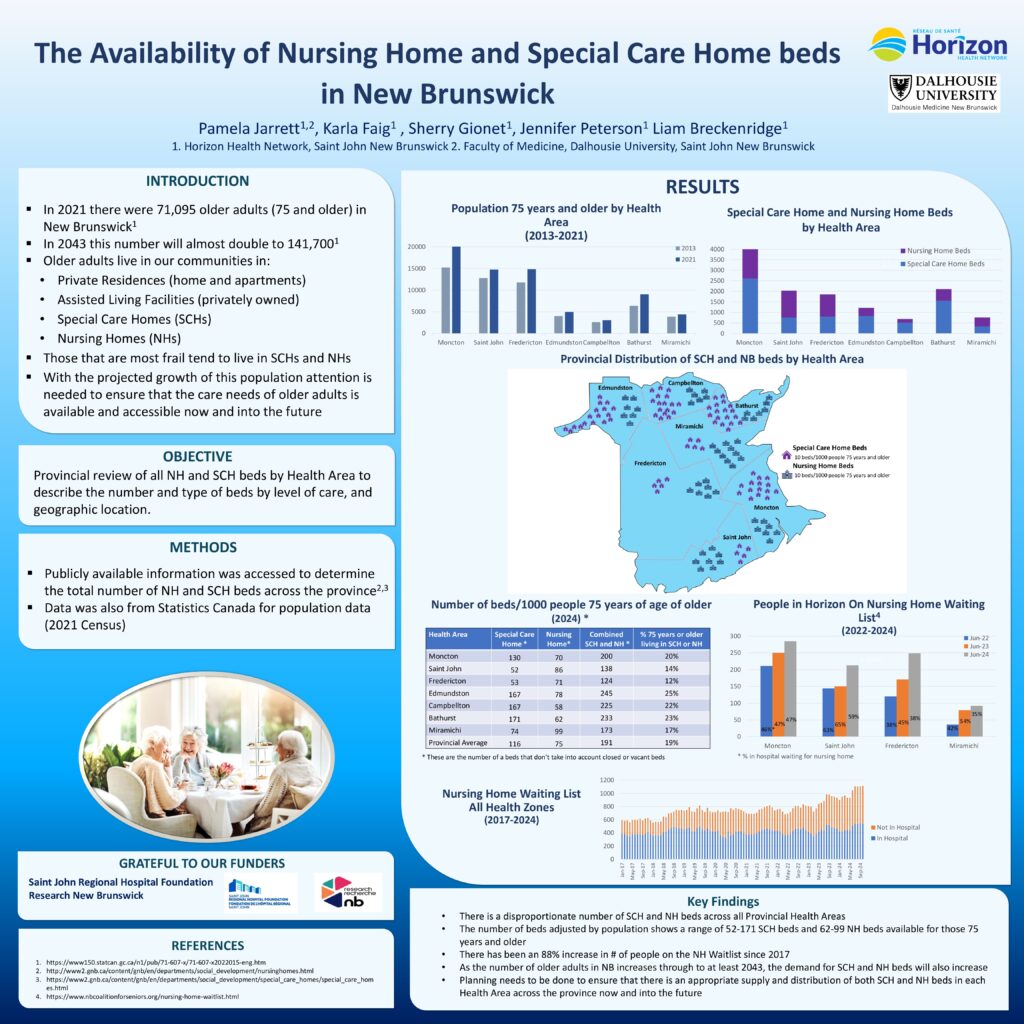
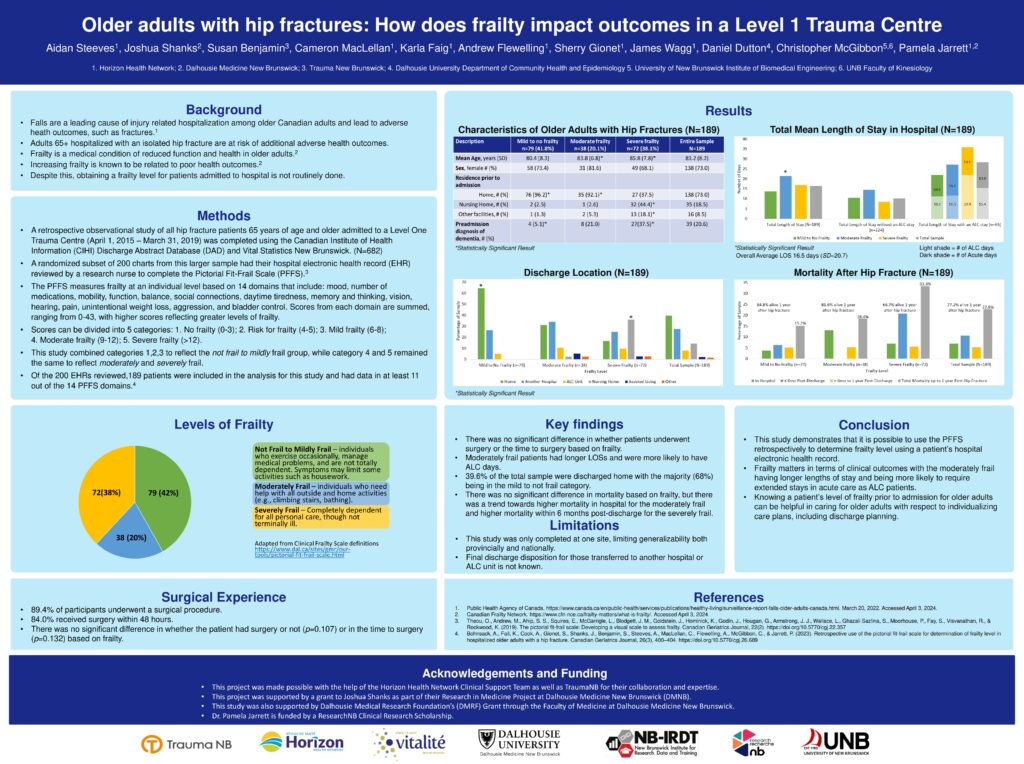
MacLellan, C., Faig, K., Cooper, L., Benjamin, S. ., Shanks, J. ., Flewelling, A. J., Dutton, D. J., McGibbon, C., Bohnsack, A., Wagg, J., & Jarrett, P. (2024). Health Outcomes of Older Adults after a Hospitalization for a Hip Fracture
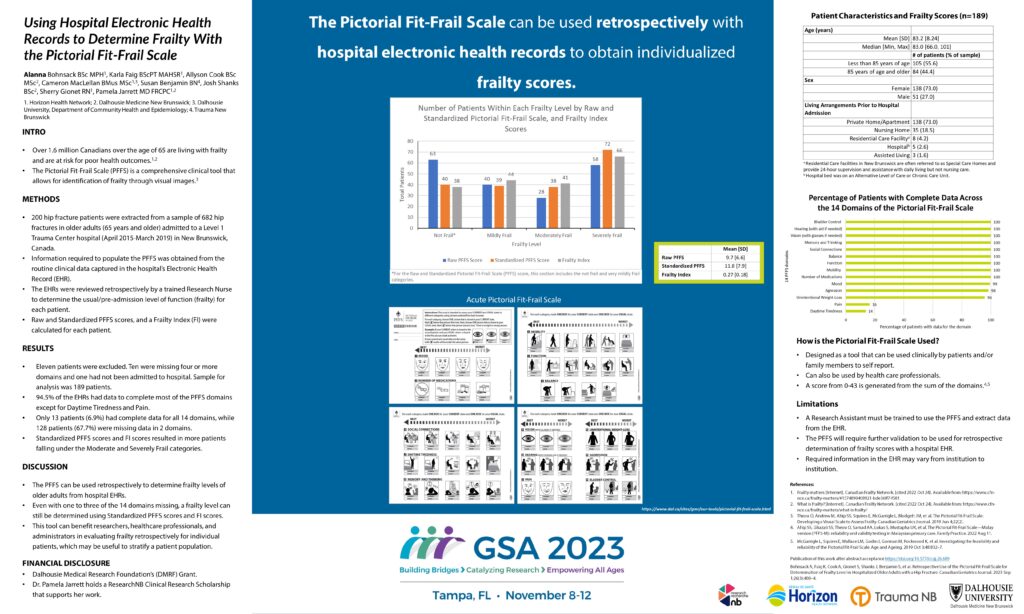
Bohnsack, A., Faig, K. ., Cook, A., Gionet, S., Shanks, J., Benjamin, S., Steeves, A. ., MacLellan, C., Flewelling, A. ., McGibbon, C., & Jarrett, P. (2023). Retrospective Use of the Pictorial Fit-Frail Scale for Determination of Frailty Level in Hospitalized Older Adults with a Hip Fracture.
Chisholm A., Ouelett L., Pishe T., Ringuette J., Watson I. (2021). Are early specialist consultations helpful predictors of those who require care in level 1 or 2 designated trauma centres? TAC. (Award-winning oral abstract)
Benjamin S., McEachern S., Watson I. (2021). Was the introduction of a provincially standardized consensus statement for postintubation analgesia and sedation associated with increased use of associated pharmacological therapies in New Brunswick? TAC. (Award-winning poster abstract)
Benjamin S., Watson I. (2021). Are there important variations in the care of adult trauma patients with isolated, nonoperative subdural hematomas between those admitted to a neurosurgical centre and those admitted to a non-neurosurgical centre for their entire inpatient stay? TAC.
Benjamin S., Chisholm A., Ouelett L., Totton L., Vautour J., Watson I. (2021). Is the use of business intelligence software helpful in planning injury prevention campaigns? TAC.
McEachern S., Ringuette J., Watson I. (2021). Exposure to endotracheal intubation among trauma patients in level 5 trauma centres in New Brunswick — a retrospective review. TAC.
Hickling A., Mallory K.D., Wilson K.E. et al. (2020). The youth concussion awareness network (You-CAN) – a school-based peer-led intervention to improve concussion reporting and social support: the protocol for a cluster randomized trial. BMC Public Health 20, 186.
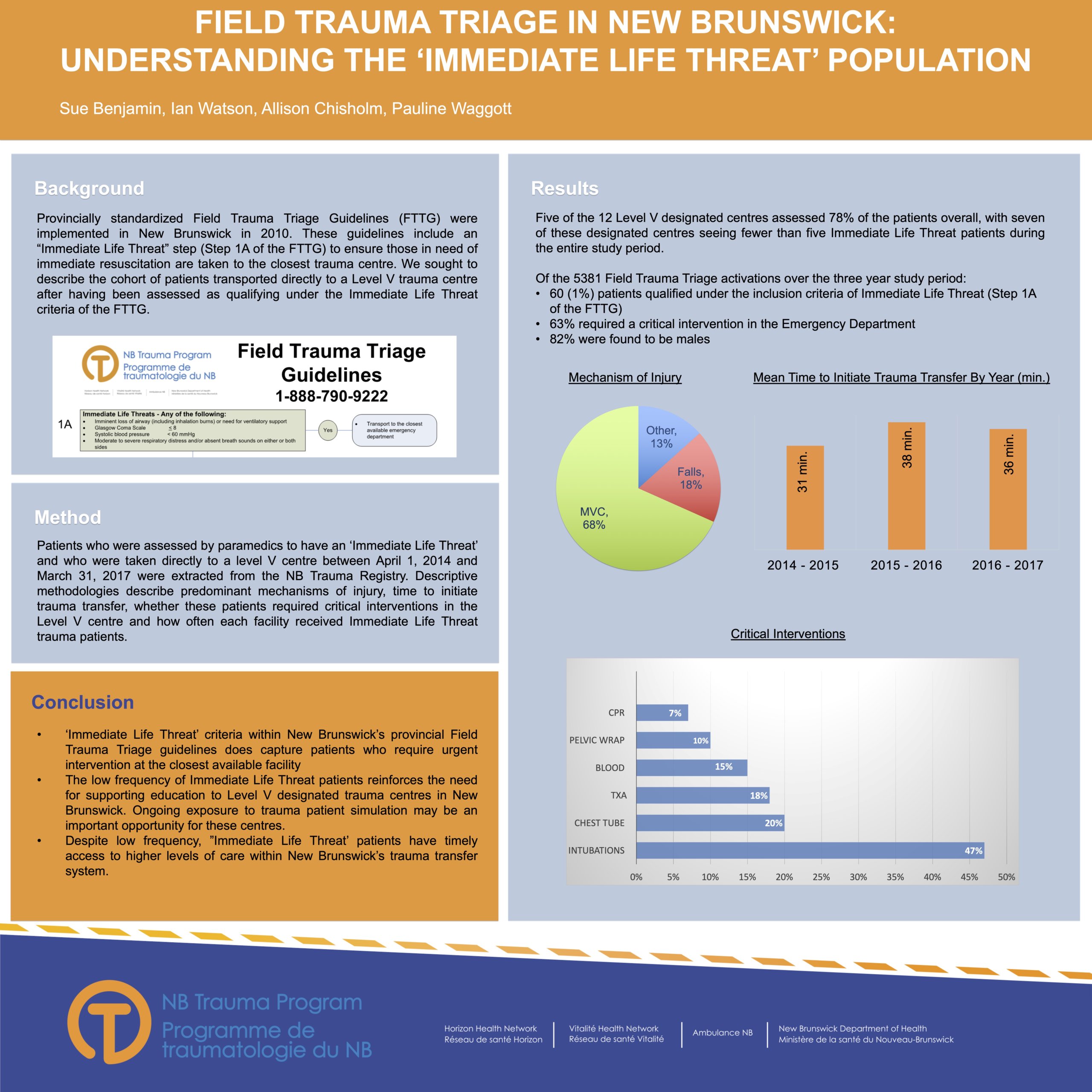
Benjamin S., Chisholm A., Watson I. (2019). Field trauma triage in New Brunswick: Understanding the “Immediate Life Threat” population TAC
Benjamin S., Chisholm A., Watson, I. (2019). What are the characteristics of field trauma triage “Bypass Failures” in an integrated, inclusive provincial trauma system? TAC
Hanlon R., French J., Atkinson P., Fraser J., Benjamin S., Poon (2019). Designing team success – an engineering solution to avoid chest tube equipment chaos using best available evidence, consensus and prototyping. Abstract Journal Canadian Journal of Emergency Medicine; 21(S1):S52
Hanlon R., French J., Atkinson P., Fraser J., Benjamin S., Poon (2019). Designing team success – an engineering approach to capture team procedural steps to develop microskills for interprofessional skills education: Abstract Journal Canadian Journal of Emergency Medicine; 21(S1):S85-86
French J., Maclean D., Fraser J., Benjamin S., Atkinson P. (2018). P050: How aware is safe enough? Situational awareness is higher in safer teams doing simulated emergency airway cases. Can J Emerg Med, 20(S1), S74-S74.
French J., Maclean D., David K., McCoy A., Benjamin S., Fraser J., Pishe T., Atkinson P. (2018). P049: Changes in situational awareness of emergency teams in simulated trauma cases using an RSI checklist. Can J Emerg Med, 20(S1), S74-S74.
French J., David K., Benjamin S., Fraser J., Mekwan J., Atkinson P. (2018)MP19: Interprofessional airway microskill checklists facilitate the deliberate practice of direct intubation with a bougie and airway manikins. Can J Emerg Med, 20(S1), S47-S47.
French J., David K., Benjamin S., Fraser J., Mekwan J., Atkinson P. (2018). Interprofessional airway microskill checklists facilitate the deliberate practice of surgical cricothyrotomy with 3-D printed surgical airway trainers. Can J Emerg Med, 20(S1), S73-S74.
Hayre J., Rouse C., French J., Fraser J., Watson I., Benjamin S., Chisholm A., Stoica G., Sealy B., Erdogan M., Green R., Atkinson P. (2018).A traumatic tale of two cities: A comparison of outcomes for adults with major trauma who present to differing trauma centres in neighbouring Canadian provinces. Can J Em Med 20(2); 191-199.
Watson I., Benjamin S., Chisholm A., Ellis K., Pishe T. (2018). Rollover motor vehicle crashes in New Brunswick: A descriptive study. Can J Surg 61 (2 Supp 1) S9.
Watson I., Ellis K., Chisholm A., Pishe T. (2018). Does the presence of CT scanning in level V centres delay access to defintive care? A retrospective review from New Brunswick’s inclusive trauma system. Can J Surg 61 (2 Supp 1) S9.
Benjamin S., Watson I., Chisholm A., Pishe T. (2018). An evaluation of overtriage in New Brunswick’s field trauma triage system. Can J Surg 61 (2 Supp 1) S9.
Benjamin S., Watson I., Chisholm A., Pishe T. (2018). Major trauma and field trauma triage in New Brunswick. Can J Surg 61 (2 Supp 1) S10.
Benjamin S., Atkinson P., Fraser J., French J. (2018). How aware is safe enough? Situational awareness is higher in safer teams doing simulated emergency airway cases CJEM; 20(Supp1):S74
Robinson B., Ellis K., Holland M., Chisholm A., Watson I. (2018). Building a model for assessing trauma-related mortality in a rural trauma system. Can J Surg 61 (2 Supp 1) S10.
Rouse C., Hayre J., French J., Fraser J., Watson I., Benjamin S., Chisholm A., Sealy B., Erdogan M., Green R.S., Stoica G., Atkinson P. (2018). A traumatic tale of two cities: does EMS level of care and transportation model affect survival in patients with trauma at level 1 trauma centres in two neighbouring Canadian provinces?” Emerg Med J., 35(2): 83 – 88.
2017
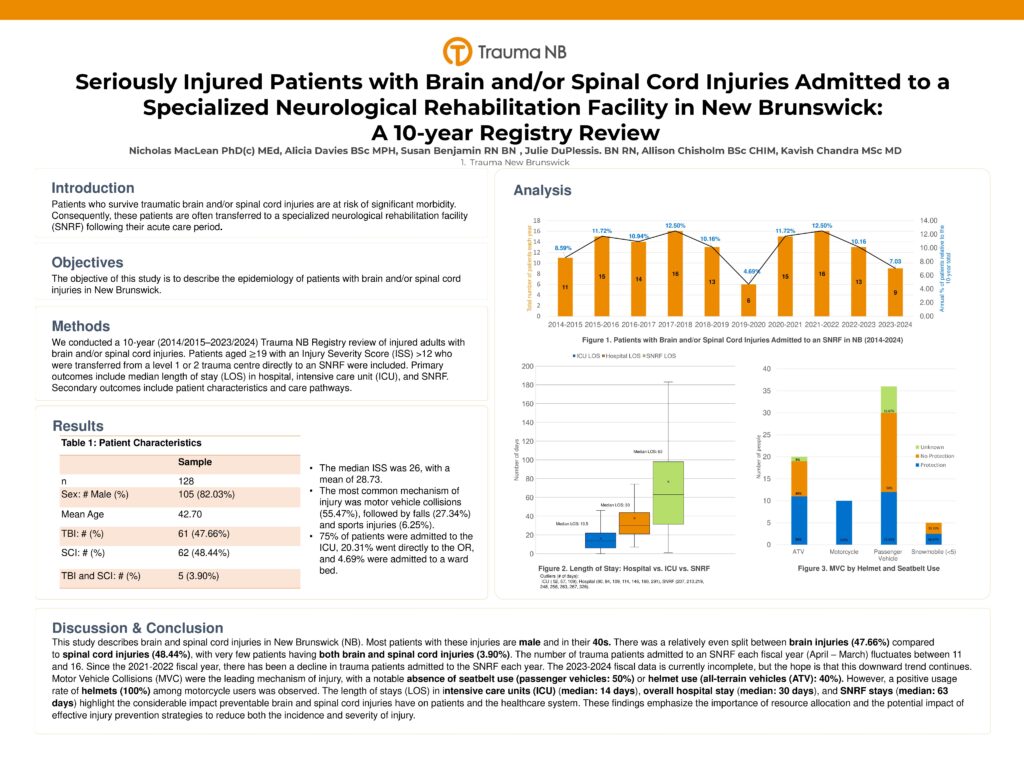
2016/2017 TPRF Award Winner – Dr. Neil Branch, Dr. Pamela Jarrett, Dr. James Wagg, Dr. Tushar Pishe, Ian Watson, Sue Benjamin, Dr. Linda Yetman, Dr. Bryn Robinson, Dr. Dan Crouse, Dr. Chris McGibbon & Allison Chisholm for the study: Outcomes in Older Adults with Isolated Hip Fractures: A Comprehensive Study across Regional Hospitals in New Brunswick
Benjamin S., Chisholm A., Watson I., Pishe T. (2017). Understanding clinical hip fracture variation in New Brunswick. Can J Surg 60 (3 Supp 2) S23.
Louis R., Benjamin S., Chisholm A., Pishe T., Watson I. (2017). Concussion and admission diagnosis among seniors who fall: A descriptive analysis. Can J Surg 60 (3 Supp 2) S32.
2016
2015/2016 TPRF Award Winner – Dr. James French, Jacqueline Fraser & Devon McLean for the study: Does the use of an RSI checklist and equipment silhouette in simulated emergency scenarios improve team performance and operational safety?
McLean D., French J., Fraser J., Benjamin S., Atkinson P. (2016). Does the use of an RSI checklist and equipment silhouette in simulated emergency scenarios improve team performance and operational safety? Can J Surg 59 (3 Supp 1) S18.
Benjamin S., Hogan A., Watson I., French J. (2016). Exposure to major trauma patients and safety-critical procedures. Part 1: Risk and reliability. Can J Surg 59 (3 Supp 1) S18.
Orchard J., Cormier C., Chisholm A., French J., Pishe T., Watson I. (2016). Impact of a pre-alert program for air ambulance response to major trauma patients in a provincial, inclusive trauma program: The New Brunswick experience. Can J Surg 59 (3 Supp 1) S19.
Woodford S., Hogan A., Watson I. (2016). Impact of the repeated offering of the Rural Trauma Team Development Course (RTTDC) on trauma transfer intervals in a provincial, inclusive system. Can J Surg 59 (3 Supp 1) S19.
Kenney M., French J., Fraser J., Phlean of Emer B., Watson I., Benjamin S., Chisholm A., Atkinson A. (2016). Out in the sticks and stones may break your bones, but does rurality surely hurt you? Trauma patient health equality in New Brunswick. Can J Surg 59 (3 Supp 1) S19.
Benjamin S., Hogan A., Chisholm A., Watson I. (2016). The timely use of tranexamic acid in trauma. Can J Surg 59 (3 Supp 1) S20.
2015
2014/2015 TPRF Award Winner – Dr. Grant Hanigan, Dr. Gabriel Cormier, Dr. Mathieu Bélanger & Dr. Alier Marrero for the study: Validation of a novel tool, the RT2, for clinical diagnostic accuracy of falls occurrence in persons with Multiple Sclerosis
Phelan B., Fraser J., Pishe T., Middleton J., Chisholm A., Benjamin S., Watson I., Atkinson P. (2015). Severe trauma in the province of New Brunswick: A descriptive epidemiological study. Can J Em Med 17 (Supp1) s77.
Chisholm A., Benjamin S., Hogan A., Woodford S., Watson I. (2015). All in the family: Creating and implementing an inclusive provincial trauma registry. Can J Surg 58 (2 Supp 1) S18.
Hogan A., Woodford S., Watson I. (2015). Lessons learned from a provincial trauma transfer system. Can J Surg 59 (3 Supp 1) S18-S19.
Watson I., Hogan A., Woodford S., Chisholm A., Louis R., St. Pierre E. (2015). Trauma NB : 5 years later. Can J Surg 59 (3 Supp 1) S19.
Hogan A., Louis R. (2015). Provincial coordination of injury prevention: The New Brunswick experience. Can J Surg 59 (3 Supp 1) S19.
Hogan A., Woodford S., Watson I. (2015). Improving access and uptake of Trauma Nursing Core Course (TNCC): A provincial approach. Can J Surg 59 (3 Supp 1) S19.
Hewitson L., Atkinson P., Mekwan J., Verbeul G., Lewis D. (2015). ULTRASIM : Ultrasound in trauma simulation. Does the use of ultrasound during simulated scenarios imrpive diagnostic abilities ? Can J Surg 59 (3 Supp 1) S19-S20.
Rouse C., Hayre J., French J., Watson I., Benjamin S., Fraser J., Chisholm A., Sealy B., Erdogan M., Green R., Atkinson R. (2015). Traumatic tale of 2 cities part I: Does being treated by different EMS affect outcomes in trauma patients destined for transport to level I centres in Halifax and Saint John? Can J Surg 59 (3 Supp 1) S20.
Rouse C., Hayre J., French J., Watson I., Benjamin S., Fraser J., Chisholm A., Sealy B., Erdogan M., Green R., Atkinson R. (2015). Traumatic tale of 2 cities part II: Does being treated by different hospitals affect outcome in trauma patients destined for transport to level I centres in Halifax and Saint John? Can J Surg 59 (3 Supp 1) S20.
Phelan B., Fraser J., Pishe., Middeton J., Chisholm A., Benjamin S., Watson I., Atkinson P. (2015). Severe trauma in the province of New Brunswick: A descriptive epidemiological study. Can J Surg 59 (3 Supp 1) S28.
2014
2013/2014 TPRF Award Winner – Dr. Paul Atkinson & Dr. James French for the study: Tranexamic acid for the treatment of significant traumatic brain injury: an international randomized, double blind placebo controlled trial.
Atkinson P., French J., & Nice C. A. (2014). Procedural sedation and analgesia for adults in the emergency department. BMJ, 348(9), 2965-2977.
Exposure to major trauma management of learners training to become emergency physicians in New Brunswick. Can J Surg 57 (3 Supp 3) S65-S66.
Montazeri R., Wagg J., Mayich J., King H., Swan J., Fraser J., Benjamin S., Atkinson P. (2014). Distal radial fractures: Adequacy of reductions performed in the emergency department. Can J Surg 57 (3 Supp 3) S75.
Boulay R., Richard D., Savoie J-P., Goulette E., Chisholm A., Watson I. (2014). Improving effectiveness of field trauma triage activations in New Brunswick. Can J Surg 57 (3 Supp 3) S75-S76.
Benjamin S., Chisholm A., Watson I. (2014). Field trauma triage guidelines as a predictor of key emergency department time intervals. Can J Surg 57 (3 Supp 3) S76.
2013
2012/2013 TPRF Award Winner – Dr. Leanne Hewitson, Dr. Paul Atkinson, Dr. Glen Verheul & Dr. David Lewis for the study: ULTRASIM: Ultrasound in TRAuma SIMulation. Does ultrasound simulation improve diagnosis during simulated scenarios?
Hogan A. (2013). Sport related concussion care in the emergency department: What every ED nurse needs to know. Can J Em Nursing 36:2; 22-23.
Atkinson P., Fraser J., Benjamin S., Sproul E., Mehta A. (2013). Wake up: Head injury management around the clock. Can J Em Med (15 Supp 1) S22.
Hogan A. (2013). A collaborative approach to reducing injuries in New Brunswick: Acute care and injury prevention. Can J Surg 56 (2 Supp) S27.
Watson I., Boulay R., Chisholm A., Beairsto E., Goulette E., Martin M. (2013). Impact of changes to a provincial field trauma triage tool in New Brunswick. Can J Surg 56 (2 Supp) S28.
Woodford S., Benjamin S., Boulay R., Watson I. (2013). Ensuring quality of field trauma triage in New Brunswick. Can J Surg 56 (2 Supp) S28.
Hogan A., Boulay R., Watson I. (2013). Benefits of a provincial trauma transfer referral system: Beyond the numbers. Can J Surg 56 (2 Supp) S28.
Boulay R., Watson I., Savoie J., Benjamin S., Martin M. (2013). The field trauma triage landscape in New Brunswick. Can J Surg 56 (2 Supp) S28-S29.
Watson I., Hogan A., Woodford A., Benjamin S., Chisholm A., Ondiveeran H., Martin M. (2013). Impact of Rural Trauma Team Development Course (RTTDC) on trauma transfer intervals in a provincial, inclusive trauma system. Can J Surg 56 (2 Supp) S29.
Howlett M., Atkinson P., Doody K., Fraser J., Leblanc-Douchin D., Strack B. (2013). Trauma and stress: A critical dynamics study of burnout in trauma centre healthcare professionals. Can J Surg 56 (2 Supp) S29.
Atkinson P., Naveed A., vanRensburg L., Madan R. (2013). Ultrasound-guided pediatric forearm fracture reduction in the emergency department. Can J Surg 56 (2 Supp) S29.
Chesters A., Atkinson P. (2013). Block first, opiates later? The use of fascia iliaca black for patients with hip fractures in the emergency department: A systematic review. Can J Surg 56 (2 Supp) S29-S30.
Atkinson P., Fraser J., Verheul G., Parks A., Milne J. (2013). Simulation in trauma ultrasound training. Can J Surg 56 (2 Supp) S30.
Fraser J., Atkinson P., Benjamin S., Sproul E., Mehta A. (2013). Wake up: Head injury management around the clock. Can J Surg 56 (2 Supp) S31.
2012
Musgrave E. (2012). Trauma NB : A model of inclusivity. Outlook 35(1); 23-24.
Benjamin S., Hogan A. (2012). Closing the quality improvement loop: A collaborative approach. Can J Surg 55 Supp, S23.
Hogan A., Benjamin S. (2012). National Trauma Registry: “Collecting” it all in New Brunswick. Can J Surg 55 Supp, S23.
Fraser J., Atkinson P., Benjamin S. (2012). Does delay to initial shoulder reduction attempt affect success rate for anterior shoulder dislocation (pilot study)? Can J Surg 55 Supp, S23.
Martin M., Watson I, Hogan A., Benjamin S., Woodford S. (2012). Use of multidisciplinary, multi-site morbidity and mortality rounds in a provincial trauma system. Can J Surg 55 Supp, S23 –S24.
Collaborative Research
Click on the works below to access research published in collaboration with members of Trauma NB: